Urinary Incontinenceand Biofeedback
Urinary Incontinence in Women
Urinary incontinenceis the uncontrolled leakage of urine and causes significant social and hygienic problems in patients. It is very difficult to calculate the true proportion of women with urinary incontinence in our society, because many women see this problem as a normal consequence of childbirth or advancing age, and do not seek treatment or are ashamed to tell a doctor. It is thought that approximately 1/3 of all postmenopausal women complain about this problem.
Hereditary causes of urinary incontinence include advancing age, excess birth, being overweight, constipation, smoking, previous uterine surgeries, fistulas, and some medications.
Types of urinary incontinence in women:
- Stress urinary incontinence: It is the involuntary leakage of urine that occurs during activities that increase intra-abdominal pressure, such as laughing, sneezing, coughing, and exercising. It is the most common cause of urinary incontinence in women and develops because of laxity of the pelvic floor muscles.
- Urge urinary incontinence: It develops because of various stimuli causing spontaneous bladder contractions. In these patients, urinary incontinence is encountered before reaching the toilet as soon as the need to go to the toilet is felt. In most patients, the cause is unknown.
- Mixed urinary incontinence: It is urinary incontinence in which both stress type and urge urinary incontinence are seen together.
- Overflow urinary incontinence: It is due to excessive stretching of the bladder. When urine accumulates in the bladder above its capacity; A small amount of urinary incontinence is seen without feeling the need to urinate. The patient never gets the idea that he has completely emptied the bladder. It can be seen in conditions such as diabetes, extensive pelvic surgeries, and spinal cord injuries.
- Sphincter insufficiency: It is rarely seen.
When evaluating these patients, history, physical examination, 24-hour voiding diary, complete urine, urine culture, urine remaining in the bladder after voiding (residual urine) and urodynamic tests (uroflowmetry, cystometry, pressure-flow study) are used.
Its treatment can be examined in three parts as conservative, drug, and surgical treatment. In conservative treatment, Kegel exercises, biofeedback and magnetic waves are mostly treated. In drug treatment, estrogens and anticholinergic drugs are used to prevent spontaneous contraction of the bladder. Surgical treatments are performed only in mixed type and incontinence types with sphincter insufficiency. For this purpose, many abdominal and vaginal surgery methods have been described. Their success rate is around 80% on average. The most important factor of success is choosing the right surgeon.
Urinary Incontinence in Men
Urinary incontinence is observed less frequently in men. Urinary incontinence is most caused by benign enlargement of the prostate. In this disease, which prevents comfortable urination, if it is delayed, the urinary bladder can become a bag that loses its contraction feature over time. If timely intervention is made before irreversible damage to the bladder occurs, post-operative patients can return to their normal lives without urinary incontinence. Otherwise, even if they have a successful prostate surgery, they cannot urinate or continue to leak their urine. Improper prostate and bladder neck surgeries can also cause urinary incontinence in men. It also occurs in conditions such as pelvic trauma and aging.
Urinary Incontinence in Children
Urinary incontinence is present in a significant proportion of children. Urinary incontinence can occur at night, during the day, or both. Daytime urinary incontinence is encountered in 6% of girls and 4% of boys, who have reached the age of seven. After excluding structural and neural causes, urinary incontinence is usually due to a disorder in bladder storage and/or excretory functions. This group of diseases is generally referred to as "functional voiding disorders". These disorders are:
- Urge syndrome and urge incontinence: It is characterized by the need to urinate frequently and suddenly during the day. During this time, the child resorts to some urinary retention maneuvers (squatting, crossing the legs, pressing the perineum, squeezing the penis, etc.) to prevent urinary incontinence. In this way, it tries to prevent urinary incontinence by contracting the pelvic floor muscles. If these inhibitions are not sufficient, urinary incontinence occurs, which is called urge incontinence. Typically, complaints increase in the afternoon and evening hours when attention is reduced. Urination is normal and there is usually no residual urine after voiding. The child's squeezing to avoid urinary incontinence is an event that facilitates the development of UTI. In addition, increased pelvic floor muscle activity because of self-squeezing, as mentioned before, leads to delayed large toilet and constipation. Due to occasional stool leaks due to constipation, soiling may occur in underwear.
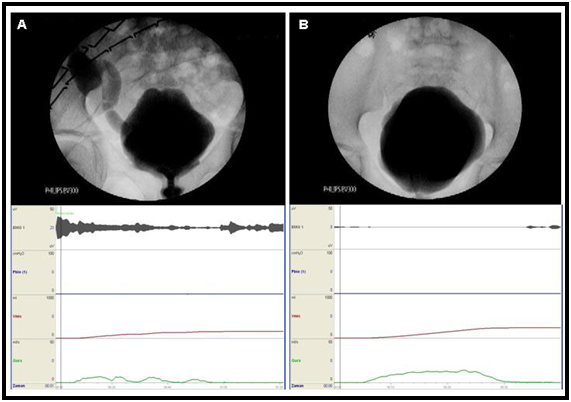
- Dysfunctional voiding: It is a condition that occurs due to contraction of the urethral sphincter and pelvic floor muscles during voiding. The most important difference of this picture from the impingement syndrome is that the normal voiding pattern is now impaired. In these children, voiding becomes intermittent, and there is usually residual urine left behind after voiding. In the later stages of this picture, the bladder muscle begins to lose its strength because the child is constantly trying to hold urine. In the uroflowmetry, voiding pattern in the form of fluctuations (staccato voiding sample) and increased EMG activity are observed in the pelvic floor electromyography (figure 1).
- Vaginal voiding: It is especially seen in fat girls who pee with their legs closed. Urine first fills the vagina, then the underwear gets wet when the child stands up.
- Giggle incontinence: In this condition, which is seen almost entirely in girls, the bladder empties suddenly and completely while laughing. The reason is not entirely clear.
How is the treatment of dysfunctional voiding done?
- Medication: If the event that triggers dysfunctional voiding is thought to be urge syndrome, anticholinergics can be added to the treatment.
- Urotherapy and biofeedback:
- Urotherapy; It is defined as a bladder training and rehabilitation program aimed at correcting the filling and voiding problems of the lower urinary system. In urotherapy, lower urinary system functions are treated with drugs and non-surgical methods. In many sources, the terms behavioral therapy, bladder training and lower urinary tract rehabilitation are also used instead of urotherapy. Biofeedback is a specific and specific form of urotherapy. Before urotherapy recommendations, it is essential that the child is given an appropriate toilet training. Good urotherapy should include the following features:
- Informing: It is very important to explain the lower urinary system function and the difference from normal to the family or the child. For this purpose, various pictures showing the normal and abnormal lower urinary tract and a balloon can be used to simulate the bladder.
- Regular (scheduled) urination: It is the conditioning of urination at 2–3-hour intervals, even if there is no feeling of urine during the day. It is important not to delay urination, not to wait until the last moment, to urinate before the feeling of urgency, and to urinate before going to bed.
- Proper (optimal) posture during voiding: Maintaining a suitable toilet posture is necessary for adequate relaxation of the pelvic floor muscles.
- Fluid intake and diet recommendations: It is recommended for most patients to increase their daily fluid intake and to reduce fluid intake in the evening and at night (especially after 6 pm). Bladder irritants are avoided: caffeine, citrus fruits, chocolate, and color-dyed drinks.
- Prevention of constipation: Sufficient fluids, food supplements and, if necessary, medications are supported.
- Support and encouragement: With the reward system, the child's self-confidence, belief, and harmony are increased.
- Biofeedback; It is the person's awareness and education with the devices placed in the body and providing information from these systems about many physiological functions of the body. For example, in urology, more information is obtained from the functions of the bladder, sphincter and pelvic floor muscles that store and empty urine, by using several devices, and it is aimed to solve the problem by concentrating on the existing problem. Children who will be treated with biofeedback should be able to distinguish the pelvic floor muscles, be well-cooperative, and have no motivation problems. Therefore, children who will be treated with biofeedback should be over 5 years old. There are types of biofeedback therapy applied using signals of different biophysiological functions (such as detrusor pressure, pelvic floor EMG activity, anal sphincter EMG and uroflowmetry).
- Cystometric (intravesical) biofeedback: It used to be applied in detrusor overactivity, it is not applied anymore.
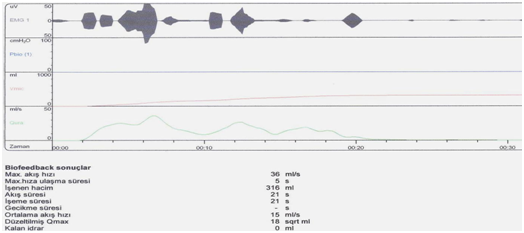
- Uroflowmetric biofeedback: During urination, the child watches the flow pattern on the monitor screen and according to the shape, the urotherapist guides the child and motivates the child to create the most appropriate flow shape (such as mountain shape or bell shape). Thus, the child receives information directly during urination and can make corrections.
- Pelvic floor electromyographicbiofeedback: The aim is to ensure the correct and effective use of the pelvic floor muscles, which play an important role in voiding control. Since it is the technique that we apply in practice, this technique will be discussed in a little more detail here. Children who will be started on biofeedback therapy should be able to distinguish the pelvic floor muscles and be well-cooperative. Therefore, children who will be treated with biofeedback should be over 5 years old. Technically, superficial pediatric electrodes are placed next to the external anal sphincter at the 3 and 9 o'clock positions and on the thigh area (figure 2).

Figure 2: Placement of superficial electrodes in a boy case
The child is seated on the uroflowmetry toilet. It is said to remain motionless and urinating until the electromyography (EMG)wave formation stabilizes. The activity of the pelvic floor muscles is recorded and reflected on the screen with EMG electrodes (figure 3).
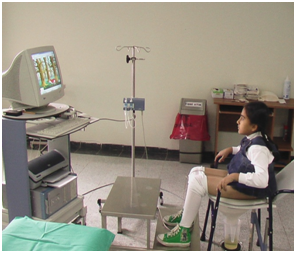
With the help of curves and shapes obtained in this way, the child can realize the pelvic floor muscles and contract and relax them in the form of a game. This training is done as an active exercise and the child is taught to relax the pelvic floor muscles during voiding as in normal voiding physiology.
Various computer animations are used in the biofeedback treatments we apply. After the animation is started, the child is told to assume that the fish or bird he sees on the screen is himself and he is asked to try to escape from the dangers (fishing rod, wolf, snake, etc.) that he encounters (figure 4 and 5). To do this, the child must adequately contract or relax the muscles in the perineum. Thus, it is aimed to teach the child to control the urinary retention muscles on his own.
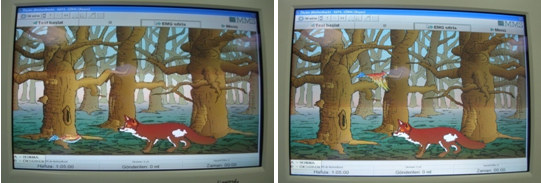
Figure 4 and 5: One of the animations we used in biofeedback treatment
6-10 sessions are required for children to learn how to isolate and relax their pelvic floor muscles. At the end of each biofeedback training, the child's uroflowmetry-EMG is taken, and the voiding curve is examined. Normally, a bell-shaped uroflowmetry curve and negative EMG activity should be obtained (figure 6).